MINNEAPOLIS — On Tuesday, White House Press Secretary Jen Psaki tweeted that the Biden administration will make sure every insured American can get reimbursed for their at-home COVID tests.
In a press release last week, the Biden administration said they will issue guidance by Jan. 15 to clarify that individuals who purchase over-the-counter COVID tests will be able to seek reimbursement.
So last week, my brother called me to let me know he had tested positive for COVID. To make sure I didn't have COVID, I purchased a COVID test kit from Walgreens. I wanted to see if that would be eligible for a reimbursement.
I spoke with health insurance navigation expert Jon Hess about the likelihood of this happening. He is the CEO of Athos Health, a health insurance navigation company.
"It's unclear right now, right now insurance companies don't have to cover it," Hess said. "The Biden administration said, by mid January they need to provide coverage for them. So there may be some out there that actually cover it, but a lot do not, and there's a lot of clarification that needs to be made about what info you need."
That being said, I called my insurance provider, Blue Cross Blue Shield of Texas (BCBSTX) to ask if I could submit a claim for my test from last week.
And the answer I got was yes! The customer service agent said the test would be covered despite the reason for the test, be it for travel, or because I showed symptoms or had a known exposure to a COVID positive patient.
All I had to do was fill out a claim form and attach a receipt.
I was able to fill out the form that I was able to download from the insurance company's website. Many insurance companies have an online portal through which you can securely communicate with them. BCBSTX let me attach my form and my receipt through that portal.
The alternative would be to fax the two things to the company, or send them via snail mail.
In terms of what kinds of tests were covered, the customer service agent said they didn't have a list of approved tests. However, added that most tests under an Emergency Use Authorization would probably pass.
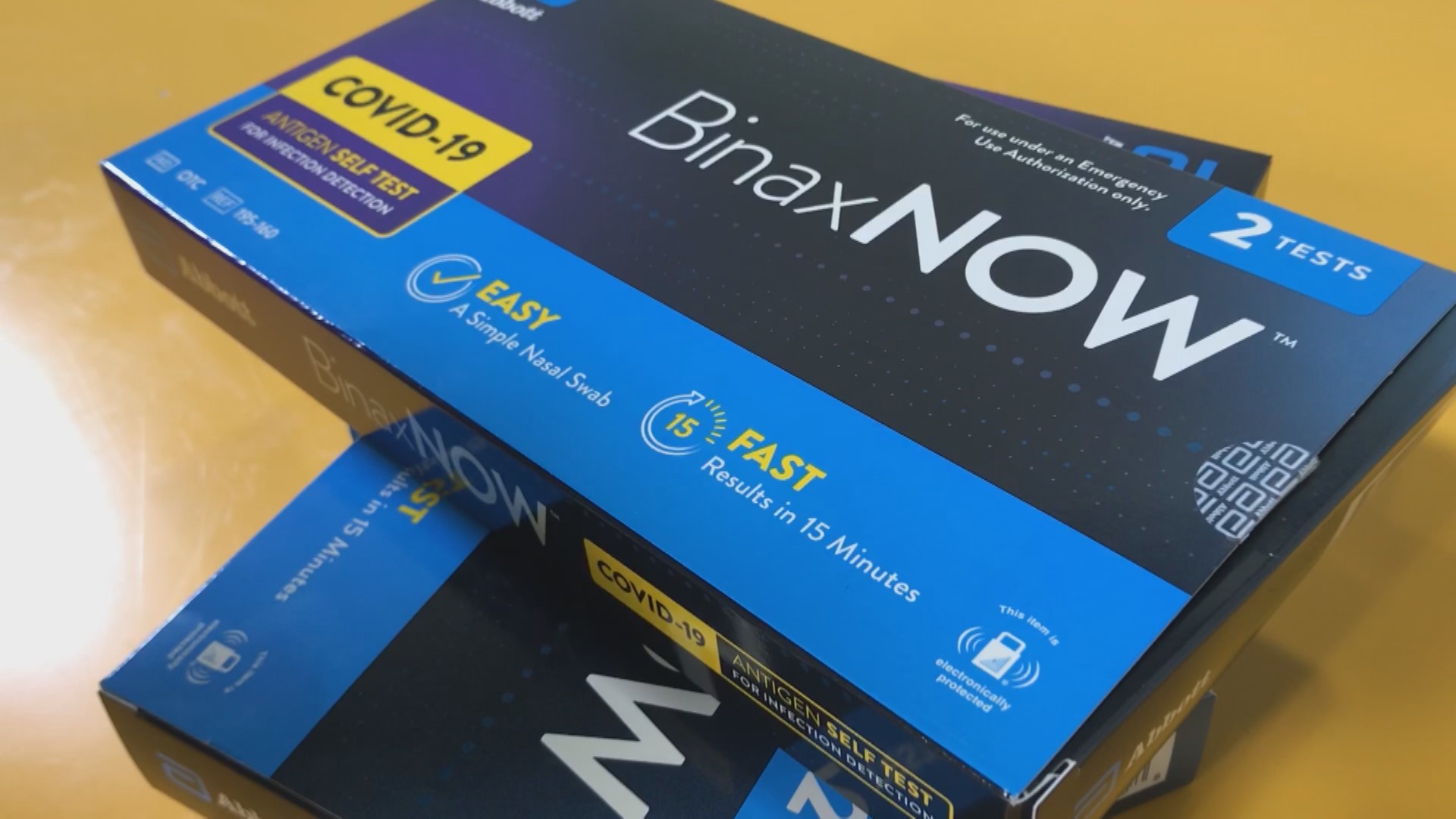
The one I submitted for review for reimbursement, BinaxNOW by Abbott has been authorized for use, under an EUA.
Hess said he was 50-50 on whether I'd be able to get my money back.
"If I was going to bet, I'd say no," he said. "It's a coin flip for me, but slightly, no, you won't get your money back."
He added that he felt that way because it's not Jan. 15 yet.
"The rules haven't been set," he said. "I think it was very clear that the Biden administration made this determination. How it's actually going to work, what the rules are haven't been communicated yet. They said they're gonna cover it, more to come mid-January."
Hess said at this point there's a bigger point worth driving home. For us here in Minnesota and Wisconsin, there is already a test that's fully covered by both the states.
The mail-in PCR saliva tests from VAULT have been approved since the beginning, and is provided to Minnesotans and Wisconsinites at no cost.
The only drawback to them is that PCR tests require a longer processing time, and an individual would have to have the foresight to order the kits beforehand, preferably before they need to be tested for COVID urgently.
"They're not as convenient, you don't get a 15-20 min read," Hess said. "But the PCR tests, which is 24 to 48 hours, that's something really good to have thinking about it for people who have school kids. [It's] free, [you] don't have to worry about reimbursement, paying anything up front, it's shipped to you. It's a great service, I don't think people take advantage of it as they could."
We reached out to several other health insurance companies and received mixed responses in terms of whether they are currently "covering" or "reimbursing" subscribers for at-home tests.
UCare's spokesperson said:
"I made a few inquiries and learned UCare covers the at-home COVID-19 tests for all plan members who have a prescription from a doctor or licensed provider. We expect federal agencies to provide guidance early next year to clarify President Biden’s expectations about broader coverage for at-home tests, and will modify our approach to meet that guidance when it becomes available."
Aetna/CVS Health said:
"Equitable access to testing has been a critical component of our pandemic response. We look forward to reviewing the guidance and adjusting our coverage policies as appropriate."