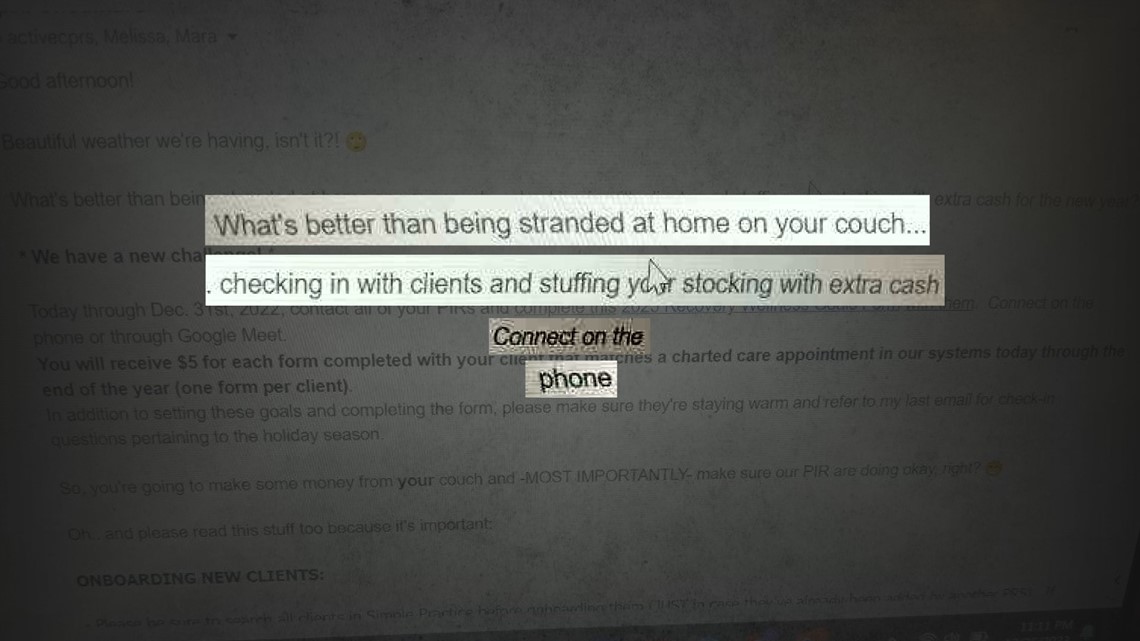
MINNEAPOLIS — “What’s better than being stranded at home on your couch checking in with clients and stuffing your stocking with extra cash for the new year??”
That was the question posed to its workers by Minneapolis-based addiction recovery company Kyros in a December 2022 email obtained by KARE 11.
It’s just one example of the questionable ways Kyros encouraged its workers to bill Medicaid for providing services to people recovering from addiction.
The email was sent to the company’s Certified Peer Recovery Specialists (CRPS), telling them to connect with all their clients on the phone or through Google Meet – despite strict limits on billing for such contacts.
Government rules prohibit billing Medicaid for most phone calls, but the Kyros email would have taxpayers footing the bill for those cash-stuffed stockings.

Peer services payments
Peer service programs are designed so that people in recovery can be paid to help mentor others battling addiction.
“So, you’re trying to help them if they relapse,” said former Kyros CPRS Tiffini Flynn Forslund. “You’re giving them support and resources, you’re mentoring them.”
Peer services are billable to Medicaid at a dollar a minute – for up to two hours a day, per client.
Kyros is Minnesota’s largest provider of peer services, according to state data reviewed by KARE 11.
The company told investors that it projected making nearly $30 million in gross profit by the end of 2024 by billing Medicaid.
Billing requirements
By law, most peer services are supposed to be one-on-one, face-to-face sessions.
Under state regulations, phone calls can be billed to Medicaid only when an appointment is made ahead of time, or if the client calls the provider in an emergency.
But when former Kyros client Daniel Schulz requested his own billing records from Kyros, he says he discovered other calls – not allowed under the rules – were billed in his name.
“Like it’s crazy!” Schulz said, as he showed his records to KARE 11.
They show Medicaid was charged $345 for nine phone calls over a three-month period.
Schulz says he didn’t make any of the calls in a crisis – and none of them were pre-scheduled appointments.
That would make the billings improper.
Misleading instructions
More than a half dozen former Kyros affiliated CPRSs, including Flynn Forslund, told KARE 11 they were never informed about the rules limiting billing for phone calls.
Instead, they say Kyros encouraged them to bill for all phone calls.

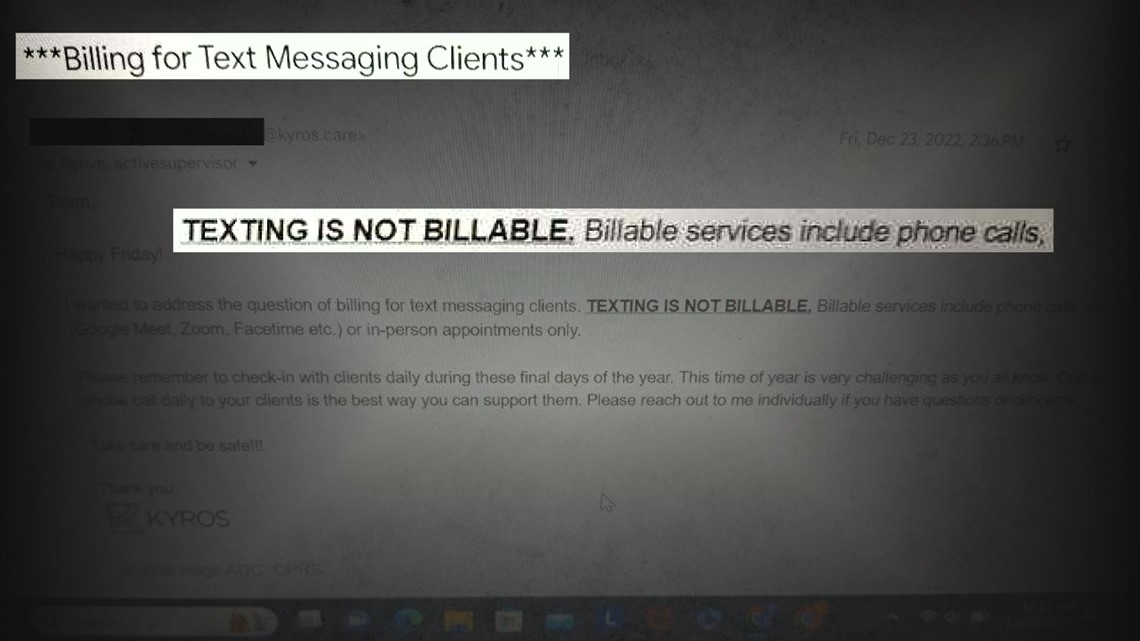
They pointed to internal emails – like the one encouraging workers to stuff their stockings with extra cash - and even the Kyros website which once instructed, “any phone call over 8 minutes qualifies” as a billable service.
The website was changed within hours after KARE 11’s first report exposing improper phone call billing.
Kyros quickly scrubbed the “any phone call” language from its website.
Policy changes
In the days following KARE 11’s investigation, Kyros insiders shared records showing the company also changed its policy.
Internal emails obtained by KARE 11 show Kyros sent new instructions to its workers about how to properly bill for phone calls.

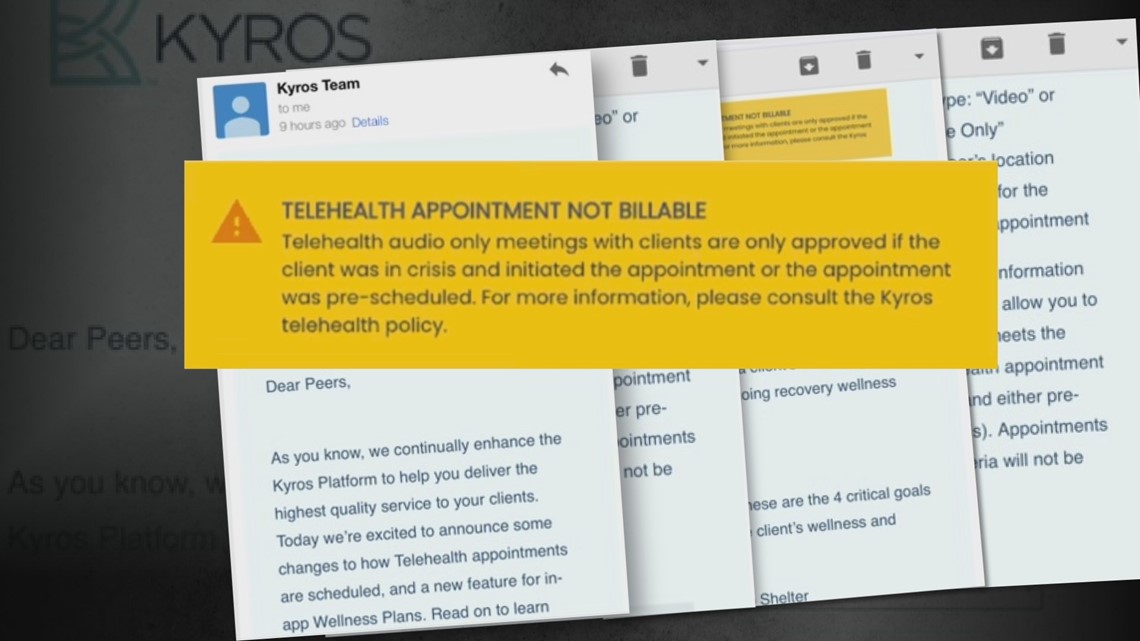
The company also rolled out a revamp of its billing platform. It added questions that specifically asked CPRS workers about the requirements that had been spelled out in KARE 11’s investigation: Was the call they’re trying to bill for prescheduled or made by the client in a crisis?
If the answers are no, the new Kyros platform instructs employees not to bill for them.
Kyros response?
Kyros has repeatedly declined KARE 11’s interview requests.
When asked in writing if Kyros was going to refund Medicaid for past inappropriate call billing, the company didn’t directly answer.
Instead, Kyros provided this response:
“Kyros has clarified its guidelines regarding billing for phone calls and reinforced the correct billing procedures with our CPRS (Certified Peer Recovery Specialists)”
Phone calls are not the only questionable billing practice KARE 11’s investigation uncovered.
KARE 11 documented how Kyros encouraged workers to take multiple clients to group events, but bill them as if they were back-to-back, one-on-one meetings – a potential violation of state and federal law.
Those group events included movie nights where taxpayers paid for Kyros peers and clients to watch hit movies.
KARE 11 obtained emails Kyros sent to its workers with instructions for a “***FREE MOVIE EVENT!!!***” at Riverview Theater in Minneapolis to watch Ant-Man and the Wasp: Quantumania.
The emails state each CPRS should bring two guests “and bill for the event!!”

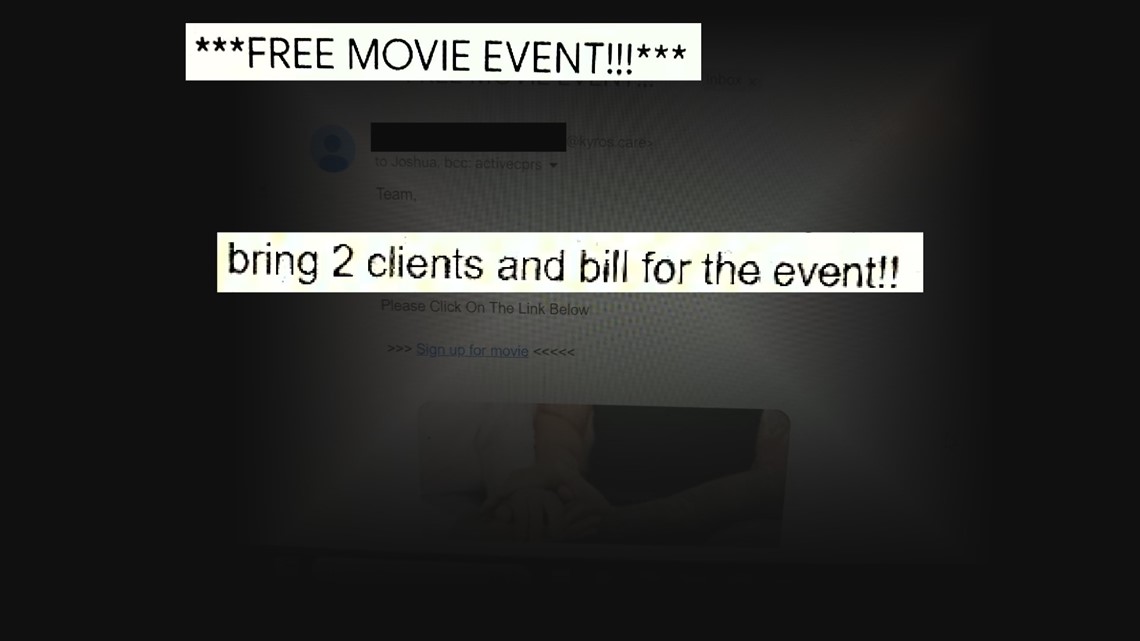
DFL State Senator John Hoffman told KARE 11 that appears to be a violation of state law which forbids group billing – and requires peer services be provided one-on-one.
“To me, by the face of this, it looks like group billing,” Hoffman said after reviewing the movie night emails.
In addition to calling for a public hearing during the upcoming legislative session, Hoffman says he’s also asked the Office of the Legislative Auditor to review how peer services have been billed to Medicaid.
When KARE 11 asked Kyros directly if they will be refunding Medicaid for its movie nights, the company responded: “Kyros trains Peers on proper regulations related to peer activities and bill accordingly.”
Since KARE 11 started reporting on the company, Kyros stripped its website of any reference to its CEO and founder Daniel Larson, who is also no longer listed on the board of the company’s non-profit partner Refocus Recovery.
Refocus and Kyros have not responded to questions about Larson’s status.
Watch more KARE 11 Investigates:
Watch all of the latest stories from our award-winning investigative team in our special YouTube playlist:

