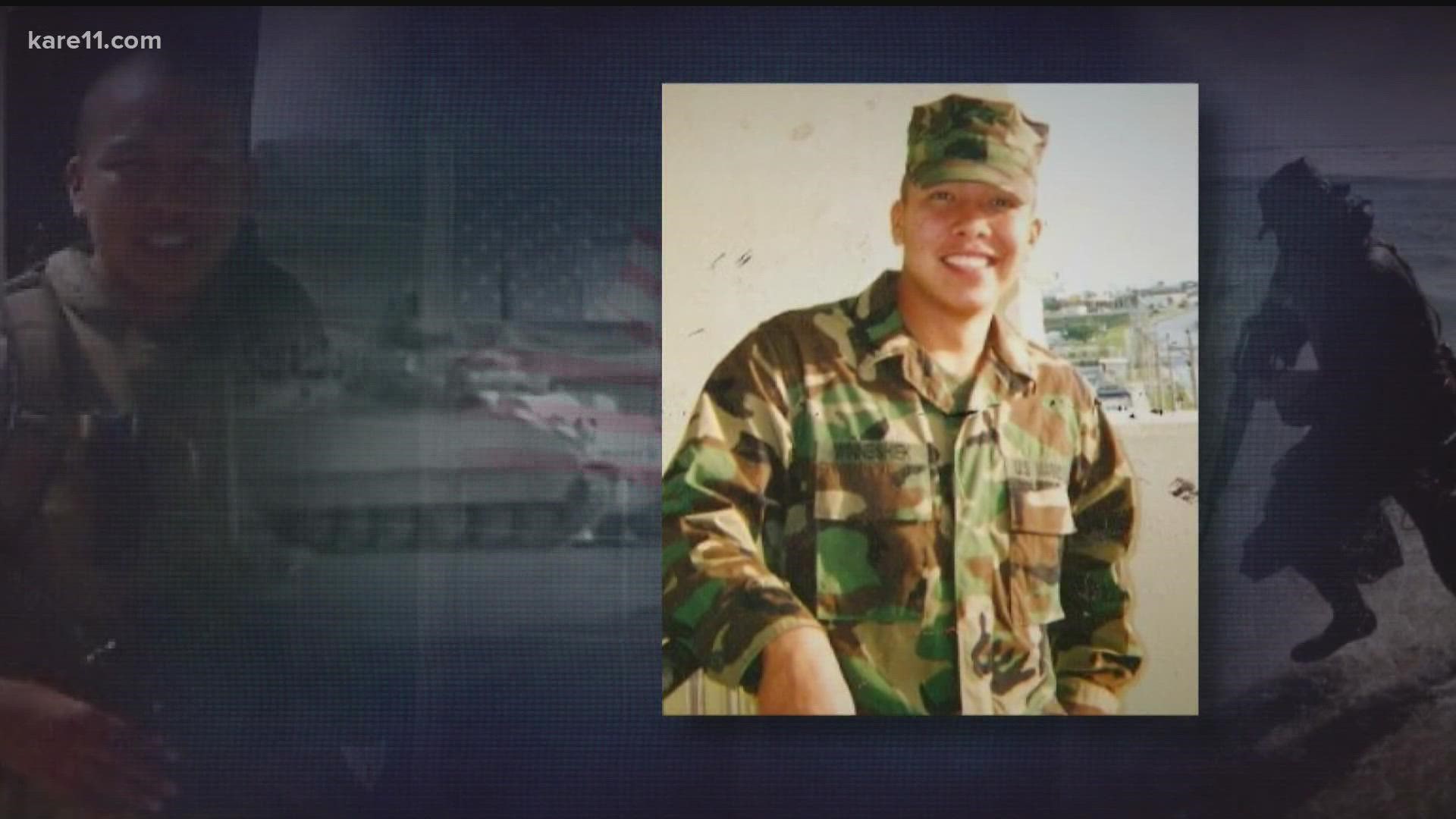
MINNEAPOLIS — “To me it feels like it happened yesterday,” said Brandon Winneshiek, infantryman and scout swimmer in the 2nd Battalion, 4th Marines.
For Brandon, the war-torn streets of Ramadi, Iraq in the spring and summer of 2004 left searing memories the passing years have not dimmed. “I’ll never forget what happened,” the veteran said.
Brandon’s unit took heavy losses, including several of his closest friends. He came home without a scratch despite at least four close calls with improvised explosive devices (IEDs) that left Marines around him wounded or dead.
What he brought back to his Wisconsin home were relentless thoughts of suicide, irritability, sudden mood changes and unexplained physical symptoms such as dizziness.
“There’s been days where I put my dress blues on – my uniform – and I’ve had a gun in my mouth and came so close to pulling the trigger,” he said.

A KARE 11 investigation finds the Department of Veterans Affairs used an unqualified doctor and inadequate testing to repeatedly deny Brandon the medical care he needed and benefits he earned when he put on his nation’s uniform, went to war, and came home with injuries.
"To get constantly denied, that's what's most upsetting," Brandon said. "That's why veterans kill themselves. My story is the perfect example."
Brandon’s Story
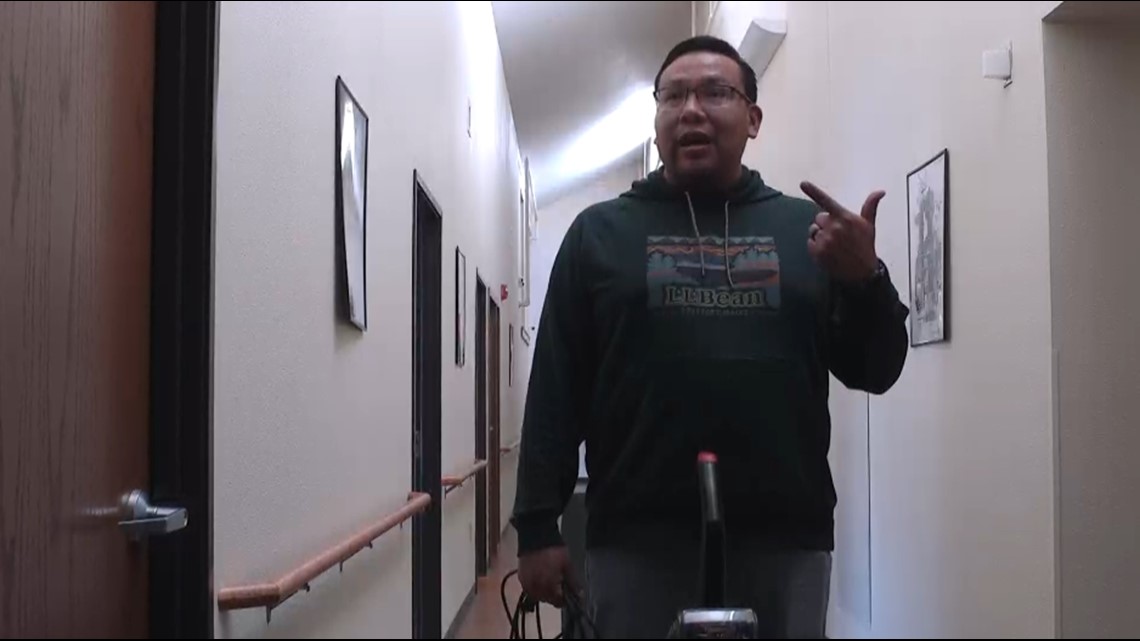
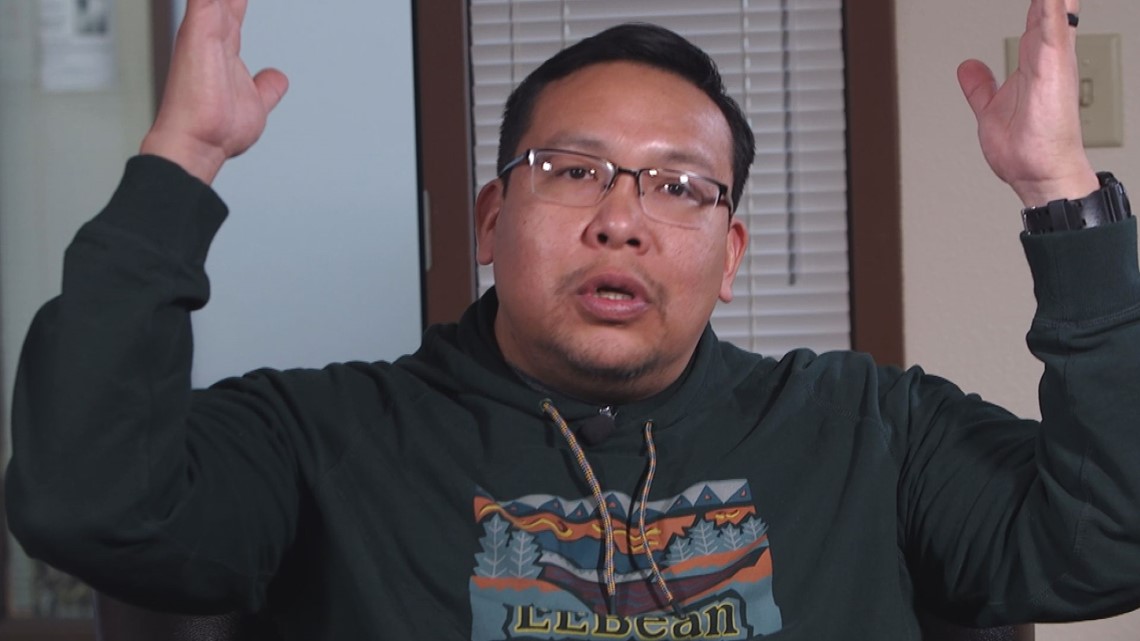
“Next thing you know – boom!” Brandon says, throwing his hands in the air as he describes a bomb placed in the stairway of a building his unit was using as a listening and observation post. “All I remember is getting up off the ground. I had been thrown across the room. My ears were ringing. I remember seeing stars and just confusion.”
Brandon’s seven-month deployment in Ramadi included three other near misses with IEDs.
One was a car bomb that went off right next to a Humvee he was riding in during a failed attempt to rescue Marines who had been cut off and were under fire. Two other IEDs exploded near him while he was on foot patrol – the blast waves knocking him off his feet. “And next thing I know, I’m picking myself up off the road, looking to make sure I had both arms and both legs,” he said while wiping away a tear.


When he first came home, Brandon says he thinks he was battling survivor’s guilt, constantly asking himself why his best friends died – and he didn’t.
Anxiety, panic attacks and nightmares became common.
“I drank,” he says of the time following his 2005 discharge from the Marines. “I drank to cope; I drank to not remember.”
“I was struggling to not kill myself,” he said.
He was diagnosed with PTSD.
In 2011, Brandon and those close to him wondered if the IED blasts also caused what has become known as the signature wound of the War on Terror – blast-related traumatic brain injury.
Records show Brandon was evaluated in early 2012 for TBI at the Minneapolis VA’s Compensation and Pension Clinic.
The doctor who did the exam acknowledged because of Brandon’s combat service, it was possible he had suffered a TBI, but wrote in his records, “I can not find any residual cognitive deficits.”
Brandon received a letter stating service connection for TBI had been denied.
What Brandon didn’t know is that he had seen a doctor who – by the VA’s own rules – was not qualified to diagnose whether a veteran had suffered a TBI.
A Nationwide Scandal
Starting in 2015, KARE 11’s Invisible Wounds investigation began exposing a pattern of veterans systematically denied a TBI diagnosis and benefits by the VA.
KARE’s investigation discovered the Department of Veterans Affairs had been using unqualified medical personnel to do examinations – and deny benefits – for traumatic brain injuries at VA medical centers nationwide.
VA rules have stated since 2008, that only highly trained doctors in one of four specialties – including neurosurgeons and neurologists – can do the initial examination to diagnose whether a veteran suffers from a TBI.
Instead of being examined by a specialist, records revealed nearly 25,000 cases across the country in which veterans were examined by doctors who were not qualified to diagnose traumatic brain injuries according to the VA’s own policy.
Minnesota Governor Tim Walz, at the time a Congressman sitting on the House Veterans Affairs Committee, demanded an official nationwide investigation of TBI claims.


There were Congressional hearings citing KARE’s reporting and the VA inspector general opened an investigation that confirmed the findings.
The Department of Veterans Affairs Secretary at the time, Robert McDonald, vowed to get the problem solved.
“We’re going through it with a fine-tooth comb nationally to make sure we get all those veterans in, and we get them what they deserve,” McDonald said in a 2016 interview.
Brandon Winneshiek’s case now raises serious questions about whether VA truly fulfilled that promise or in some cases, just moved on from unqualified doctors to inadequate exams.
Another Denial
Veterans Affairs sent letters to the nearly 25,000 veterans who had been seen by the unqualified doctors, notifying them they were eligible for a new TBI exam.
At the time, Brandon was working as a police officer for the Ho Chunk Nation in Wisconsin. He was instructed to go to the Tomah, WI VA hospital for his new exam.
His medical records show he was seen by a neurologist named Dr. Mary Jo Lanska. However, Brandon says the exam lasted just half an hour and he was told he did not have a TBI.
“How can somebody diagnose traumatic brain injury in 30 minutes? It’s impossible,” Brandon recalls thinking as he left.

Records show Dr. Lanska did no neuropsychological testing but checked “Yes” in a box claiming there were “significant diagnostic test findings and/or results.”
The records show those findings were based on her administration of a short screening test known as an MMSE – Mini-Mental State Exam. Brandon did well, scoring 28.5 out of a possible 30 points.
The MMSE is a widely used test to measure cognitive function over time among elderly dementia patients.
Videos online of the MMSE being administered show patients being asked simple questions including what day and month it is and asked to recall a series of three words.
Dr. Justin Otis, a neuropsychiatrist with Gunderson Health System, uses the MMSE in his practice. He calls it a brief screening tool.
“Are these brief screening tools adequate to diagnose traumatic brain injury?” asked KARE 11’s A.J. Lagoe.
“They are not,” Dr. Otis replied. “It’s not meant to be a diagnostic tool. It’s not sensitive or specific for traumatic brain injury.”

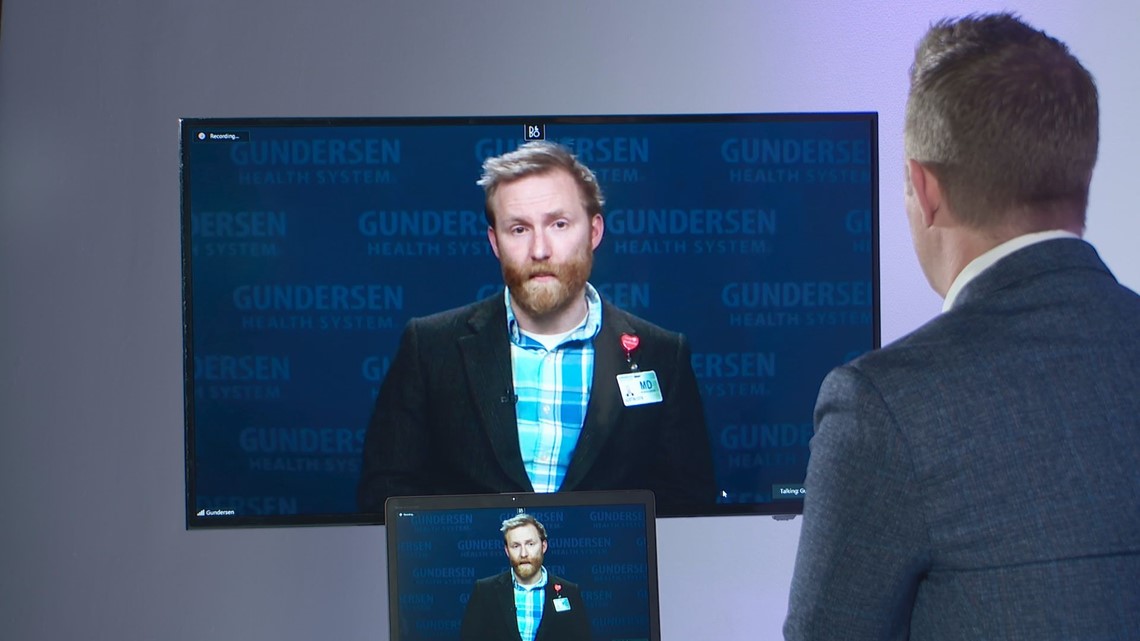
However, records show the MMSE was the only testing Dr. Lanska and Tomah VA gave Brandon before reaching the “significant diagnostic finding” that the combat Veteran did not have a TBI.
Prior Warnings About TBI Inadequate Exams
Brandon’s case is not the first time the medical community has raised concern over Veterans Affairs using inadequate testing in veteran TBI exams.
In 2015, KARE 11 profiled the case of Army Captain Charles Gatlin, who suffered a TBI in a massive car bomb attack in Kirkuk, Iraq in 2006.
The Army cited stable and permanent neurological deficits and retired Gatlin with a 70% disability. But when he applied for benefits, a VA psychologist named Dr. Robert Bateen used another type of brief screening tool called an RBANS, and determined Gatlin’s “permanent” condition had seemingly vanished.
He wrote, "If Mr. Gatlin had a cognitive impairment in the past, it is likely that this has resolved."
"I saw this man for 20 minutes," Gatlin told KARE 11. "And a decision was made."
Gatlin filed a complaint with the Montana Board of Psychologists. Ultimately, the state board sanctioned the VA psychologist. It ruled Dr. Bateen had violated "accepted standards of practice" when he based his diagnosis on the RBANS.
"It was not sensitive enough to do what the VA purported that it was supposed to do," Board Chairman Dr. George Watson told KARE 11. "So, we reprimanded the psychologist."
'Kick Rocks'
For Brandon Winneshiek, the Tomah VA’s diagnosis that he did not have a TBI meant he received no treatment specific for brain injury.
His troubles with irritability, sudden mood changes, and thoughts of suicide continued, forcing him to quit his job as a police officer and straining his marriage to his wife Josie.
“I didn’t know what to do,” Josie recalls. “Nobody is prepped as a spouse for how to handle that.”


There were also the unexplained physical symptoms including headaches and dizziness which didn’t seem to match Brandon’s diagnosis of PTSD.
“There were days when I had to wash his hair because he couldn’t keep himself upright in the shower,” Josie said.
Brandon says he continued to ask the VA for further TBI testing and continued to be denied.
“I just knew something was wrong,” he said.
In March of 2021, records show Brandon asked his primary care doctor at the Tomah VA for a consult to go outside the VA system for TBI testing.
The consult request once again landed on the desk of Dr. Mary Jo Lanska.

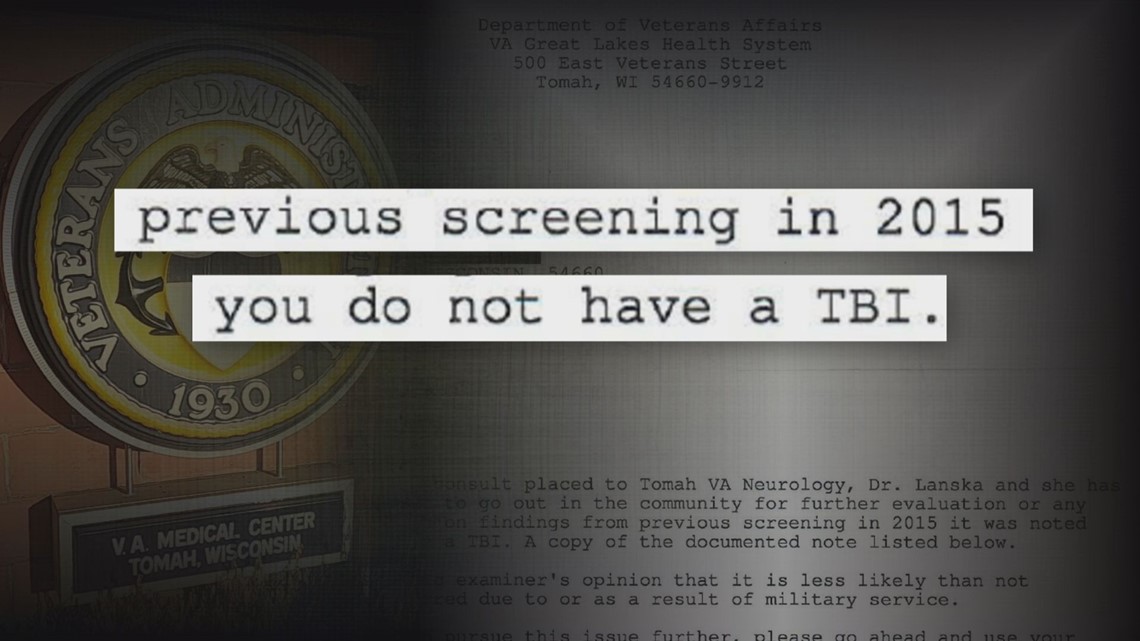
Dr. Lanska declined Brandon’s request for further evaluation. She wrote that because of her previous screening in 2015 it was noted, “you do not have a TBI.” The letter goes on to say if Brandon wanted to pursue this issue further, he could use his private insurance to get evaluated.
“The VA kicked me to the curb,” said Brandon. “Tomah VA turned me down, told me to kick rocks!”
Finally Receiving Care
Desperate for answers, Brandon turned to Gunderson Health System.
Records show he spent weeks going through a barrage of imaging and testing with multiple specialists, including Dr. Otis.
Brandon was found to have significant deficits with attention and memory and demonstrated symptoms of cognitive dysfunction consistent with a history of multiple combat-related concussions.
The specialist’s findings each pointed to the same diagnosis.
“Does Brandon have a TBI?” KARE’s Lagoe asked Dr. Otis.
“Yes,” he replied. “Brandon sustained multiple, mild traumatic brain injuries through his military career and has deficits that are, I believe to be, permanent.”
There is treatment available to help Brandon cope with the deficits of his brain injuries. And now, after a decade of denial at the VA, he’s finally getting medical care.
“It’s maddening to know that there were all these steps that could have been taken as preventative measures and as actual care for him that were missed for 10 years,” said his wife, Josie.
Presented with the evidence from his private doctors, the VA finally acknowledged that Brandon suffered traumatic brain injury during his time in the service and he’s started receiving TBI-related benefits. He’s now managing a homeless shelter for fellow veterans.
However, VA was not done issuing denials in Brandon’s case.
The Final Act of Denial
In the wake of KARE 11’s 2015 investigation exposing unqualified doctors misdiagnosing Veterans, the VA secretary announced what he called a correction to the “injustice.”
The VA’s correction was a promise of “equitable relief” for the nearly 25,000 impacted veterans.
In addition to new exams with qualified doctors, the VA promised to provide retroactive benefits to veterans who were found to have TBI back to when they first applied.
Brandon applied for that equitable relief – benefits backdated to when he first submitted his TBI claim in 2011.
He was denied.
The VA, which twice misdiagnosed Brandon – first with an unqualified doctor and a second time with an inadequate exam – now claims he is the one who screwed up.
VA states Brandon and all the other veterans were notified by letter that they only had one year after their new exam with a qualified doctor to apply for their TBI claim to be reprocessed.
Since Brandon didn’t file to re-open until years after he had a TBI diagnosis from his private doctors, VA decided his benefits can’t be back dated.
Brandon questions how he could be expected to file for benefits for an injury VA told him he didn’t even have.
“And the VA wonders why veterans are pulling into the parking lot and shooting themselves,” Brandon said.