KARE 11 Investigates: Missing records, fraud allegations, and a flawed state investigation
Minnesota Dept. of Human Services failed to fully investigate allegations of illegal billing in taxpayer-funded program to help people in addiction recovery.
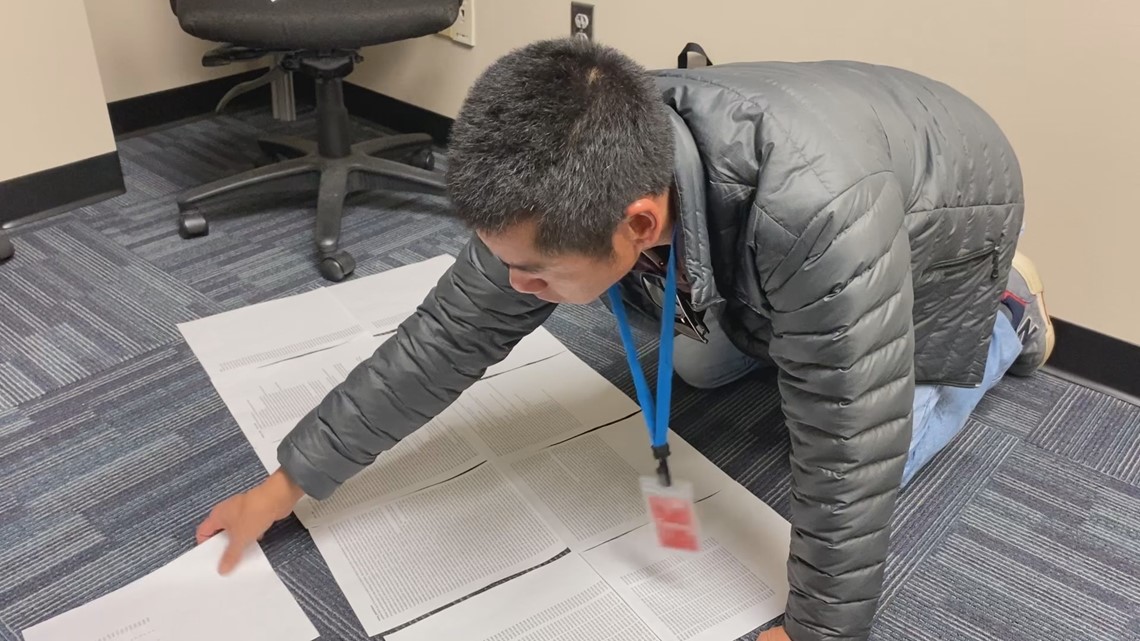
“It’s like a collage,” said Daniel Schulz as he kneeled on the floor trying to arrange his medical records.
When Schulz requested his records from Kyros, the state’s largest provider of peer recovery services, he expected the company to provide what state and federal law requires – his complete health record.
He expected information about his treatment plan and details of the services he received as he recovered from substance use disorder.
Instead, Kyros handed over what amounted to puzzle pieces – more than a dozen printed pages from a spreadsheet that he had to lay out, stretch across the floor, and tape together just to begin to be able to read the diced-up columns and rows.
Once that was done, Schulz found numerous records were missing.
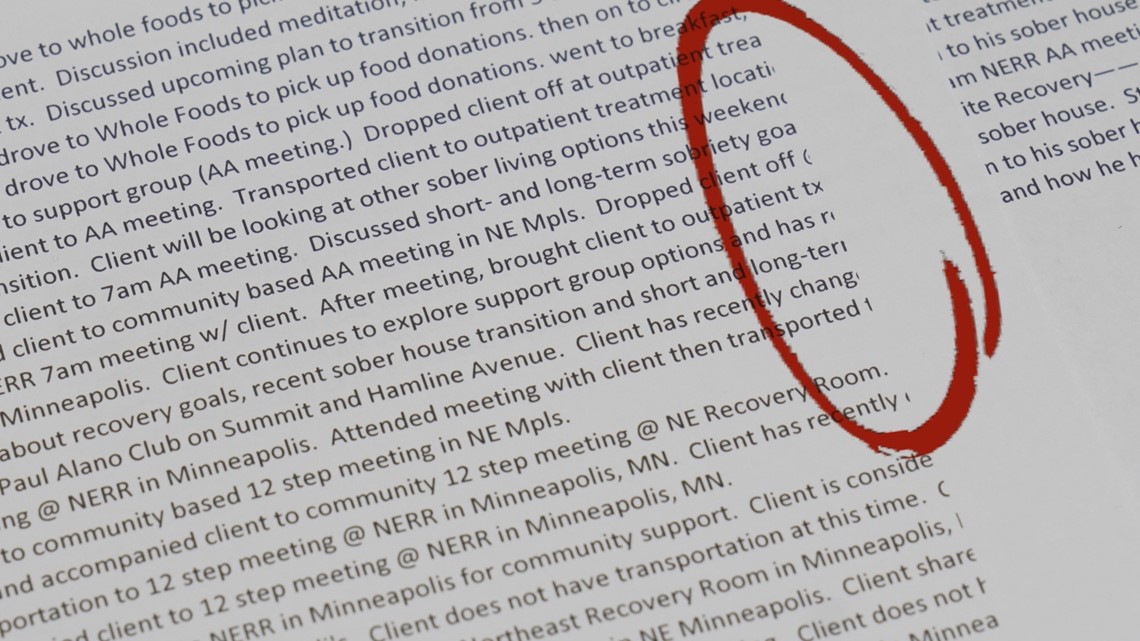
There was no record of his diagnosis or treatment plan. More than a dozen entries listed the amount billed – but had no information about what services were provided.
Entries that described services were often cut off in mid-sentence.
Still, Schulz says the information he could see concerned him.
“When you look at the records you got, in your opinion, is there false billing there?” KARE 11 Investigative Reporter A.J. Lagoe asked.
“Oh, most definitely,” Schulz replied, “Absolutely!”
It’s not the first time a client has accused Kyros of billing for services they never received.
“I’m saying that outright did not happen,” replied Aubrey Kjerstenson when KARE 11 interviewed her last year.
Chapter 1 Taxpayer-Supported Peer Recovery
Kyros and its non-profit partner, Refocus Recovery, are supposed to provide mentors who have been in recovery for a year or more to clients like Schulz and Kjerstenson.
The mentors are called Peer Recovery Specialists.
Peer services are then billed to Medicaid – the taxpayer-funded health insurer for the poor – at a rate of a dollar-a-minute for a maximum of two hours per client, per day.
For Kyros, it’s become a multi-million-dollar business.
The Kyros-Refocus partnership received more than $14 million in Medicaid payments between January 2022 and November 2023, according to state data reviewed by KARE 11.

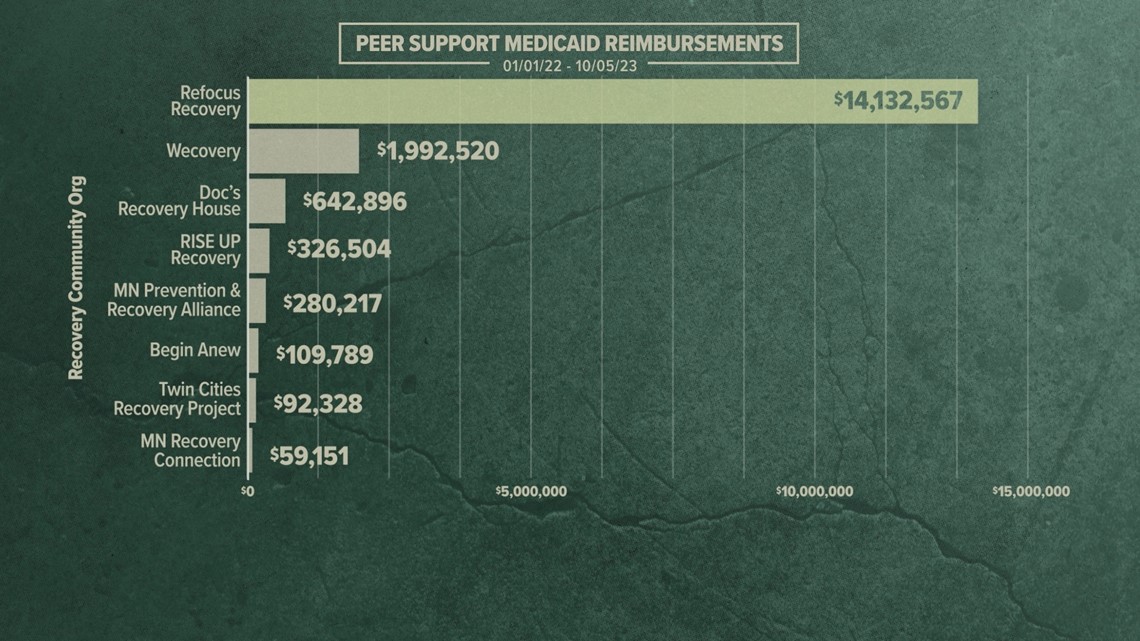
In an “Investment Overview” obtained by KARE 11, Kyros projected making nearly $30 million in gross profit by the end of 2024.
After reviewing his own records, however, Schulz believes Medicaid was billed for services he never received.
“Some of the events were just like made up,” Schulz said. “This needs to be investigated.”
What Schulz didn’t know was that Kyros and Refocus had already been investigated by the state agency that approves Medicaid funding.
But records show the investigation was incomplete and the state took little action.
Chapter 2 Early Red Flag
Under state law, Daniel Larson’s for-profit Kyros cannot bill Medicaid directly for peer services. But the non-profit he founded, Refocus Recovery, can. So, the non-profit hires the for-profit company to provide the client services.
To participate in Minnesota’s peer service payment system, the state typically requires organizations like Refocus to meet accreditation standards.
The most common standards are set by the Alliance for Recovery Centered Organizations, or ARCO, a program run by a non-profit based in Washington, D.C.
Refocus applied for accreditation in 2021, telling ARCO that all its funding came from personal and private contributions. The application said nothing about Kyros, and ARCO initially granted the accreditation.
But a year later ARCO was tipped about Refocus’ relationship with Kyros.
Citing what it called “undue influence on Refocus Recovery by Kyros, a for-profit entity,” ARCO decertified Refocus Recovery in July 2022, according to records obtained by KARE 11.
A letter explaining the decision stated: “There is a partnership in existence between Refocus Recovery and Kyros from which both entities stand to attain substantial financial gains.”
Chapter 3 Medicaid Funding in Doubt
The decision threatened to prevent Refocus from billing Medicaid – and to disrupt Kyros’ multi-million-dollar business model.
But the Minnesota Department of Human Services (DHS) granted a temporary waiver while Refocus appealed directly to DHS Commissioner Jodi Harpstead.
As the review dragged on, Refocus lost patience and threatened to sue DHS.
“If Refocus Recovery does not get any signals that things are moving more quickly, then we fear litigation will be the result,” an attorney wrote in early September.
Two weeks later, DHS gave its answer.
On September 16, 2022, Commissioner Harpstead sent a letter to a lawyer representing Refocus and Kyros, former judge and U.S. Attorney Erica MacDonald, granting certification for Refocus to keep on billing Medicaid.
Within months, records show the same state agency began getting tips about alleged improper billing – and allegations that taxpayers were being bilked.
Chapter 4 The “Investigation”
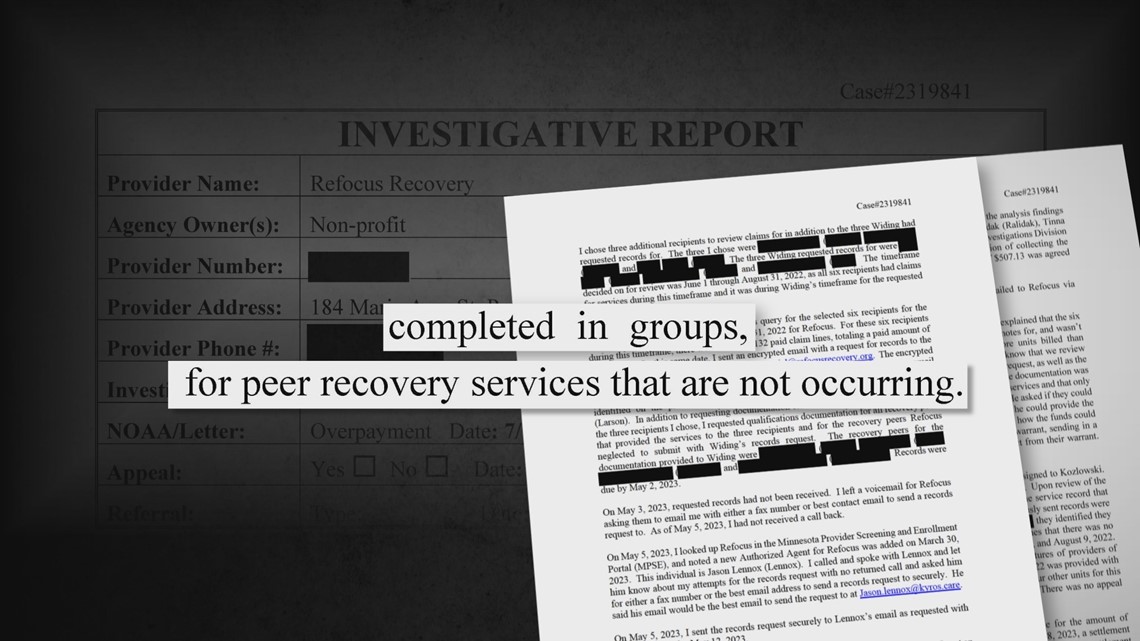
Records obtained by KARE 11 through state data practice requests show in both November of 2022, and February of 2023, DHS’s Office of Inspector General received complaints that Kyros’s nonprofit partner Refocus Recovery was improperly billing “in groups” and “for peer recovery services that are not occurring.”

“It’s critical when fraud is alleged, especially on a substantial nature like this, that a deep dive get done,” said GOP State Senator Jim Abeler in an interview with KARE 11.
KARE 11’s investigation finds DHS’s investigation was more of a toe dip than a deep dive.
After receiving the initial tip that Refocus peers were improperly billing for groups, when state law only allows one-to-one sessions, OIG investigator Stephanie Widing wrote to Refocus asking for the records of three clients.
She found Refocus was missing records for the clients, treatment plan reviews, and credentials for some Certified Peer Recovery Specialists (CPRS) when they were in question. She recommended a full case be opened.
Then, in February 2023, OIG got another tip claiming Recovery’s peers were living with clients and billing for services that never happened.
DHS investigator Benjamin Peterson picked the records of three additional clients to review.
According to a summary of the investigation Peterson sent an email requesting the records to Daniel Larson, the founder of both Refocus Recovery and Kyros, but he never responded. Another month went by. Peterson called and left a voicemail for Refocus, but no one called back.
Two days later, Peterson looked up Refocus on an internal database and saw that another person to contact would be Jason Lennox – a Kyros Vice President.
Lennox agreed to email the requested billing records – 132 out of the more than 61,800 bills Refocus had submitted by that point for Medicaid reimbursement.
His summary shows Peterson found problems in nearly 20% of the records, including missing signatures and no documentation to support whether the services billed for were actually provided.
DHS stopped its investigation there – without requesting additional records.
In a statement to KARE 11, the agency also admitted it never called any of the clients to determine if the services taxpayers were billed for were actually provided.
DHS sent Refocus a bill for $1,168 in recovery and fines. Refocus appealed and provided some of the missing records. The two sides agreed to an $850 settlement in August.
Case closed.
Chapter 5 “Asleep at the Wheel”
Because no clients were contacted, the original allegations – improper group billing and billing for services not provided – were never addressed.
“It seems like they’re asleep at the wheel,” said Sen. Abeler when provided the DHS records by KARE 11.
“My first response was, ‘that’s it,’” said DFL State Senator John Hoffman when KARE 11 asked him to also review the DHS investigative file. “I don’t think it was adequate,” he added. “There was no other follow-through, no more questions asked.”
Sen. Hoffman chairs the Human Services Committee which has oversight of DHS.
Three months after wrapping up its “investigation” DHS and Kyros joined together in November 2023 as Diamond Level sponsors at the Minnesota Association of Resources for Recovery and Chemical Health (MARRCH) conference – the state’s largest gathering of addiction treatment providers.


MARRCH’s Board of Governor’s president at the time was Amy Dellwo, Kyro’s Vice President of Strategic Policy and Growth and the former Chief of Staff for the Minnesota Department of Human Services.
KARE 11 was asked to leave the conference’s exhibit hall by MARRCH staff while recording video of the Kyros vendor booth as part of our investigation.
Chapter 6 Questionable Practices
Unlike DHS, when KARE 11 investigated, reporters began contacting current and former peer specialists and clients.
Using records they provided KARE 11 documented how Kyros and Refocus engaged in numerous questionable practices, including:
- Instructing its workers to bill for phone calls that are not allowed under state regulations.
- Allowing workers to take multiple clients to group events – like movie nights – but bill as if they were back-to-back, one-on-one meetings, a potential violation of state and federal law.
- Encouraging workers to compete for prizes and bonuses based on increasing their Medicaid billings.
Lawmakers say those are issues DHS might have uncovered if it had done a thorough investigation.
“I’m not surprised,” said Sen. Hoffman. “Because you followed the trail that a good investigator should be following, right? Follow the money.”
Daniel Larson, the founder of Kyros and Refocus Recovery, has declined multiple interview requests. But the company said in a statement: “Kyros monitors billing practices closely to ensure they meet statutory requirements, and any deviation found is addressed promptly and appropriately.”
Chapter 7 Discovering Suspicious billing
Daniel Schulz moved back home to Minnesota from San Diego to go into treatment for addictions he said were sparked by grief following the unexpected death of his father while canoeing in the Boundary Waters.
After finishing inpatient treatment at the Pride Institute, Schulz was connected in January 2023 to ACT 2 Recovery Residences which provide LGBTQIA+ sober living homes in Minneapolis.
The owner and operator of ACT 2 is Meyer Belkin.
On his first day in one of Belkin’s Minneapolis sober homes, Schulz said he was informed he needed to have “an assessment.”
“I was under the impression that my housing was contingent on this assessment,” Schulz told KARE 11, “I truly thought this assessment was to give me permission to live in one of these houses.”
The assessment, unbeknownst to Schulz, was performed by a Kyros employee, and done to sign him up for peer recovery services.
Kyros’s website lists ACT 2 sober homes as a partner, and ACT 2’s owner Belkin works for Kyros as a peer services provider.


Schulz says he discovered later that the assessment “allowed them to start charging my insurance (Medicaid) for things that I was unaware of.”
“You were receiving peer services without even knowing you were signed up for peer services?” KARE’s A.J. Lagoe asked.
“Correct,” Schulz replied. “Yeah.”
Schulz said he became suspicious when he sought out peer services from a man he’d met in treatment for help with rides to and from his outpatient program and AA meetings.
Schulz says that’s when he first learned he was already in the Kyros/Refocus system and his insurance was being billed for peer services by Belkin and others connected to ACT 2 and Kyros.
“But there were no services that had happened,” said Schulz. “So, that’s when a red flag went off.”

Chapter 8 The Grocery Runs
Schulz says he first learned the types of things Medicaid was being billed for in his name, on March 26th, 2023.
He was at breakfast with Meyer Belkin and another sober home resident.
They’d just completed what for Schulz had become a weekly occurrence – riding with Belkin in his pickup truck on Saturdays and every other Sunday to pick up groceries donated by Whole Foods and dropping them off at Belkin’s sober homes.
“He always wanted volunteers,” Schulz said. “So, I volunteered to do it.”
Schulz said during that meal Belkin told him and the other resident, that he was billing insurance for this time with both of them.
“I learned that not only was I helping him by loading the food, distributing the food, everything that went into it,” Schulz said, “he was billing my insurance for that time I was with him, helping him and his company. Free labor from me and he’s also making money from my insurance for that time.”
It was the last time Schulz helped with a grocery run and he says he moved out of Belkin’s sober home shortly thereafter.
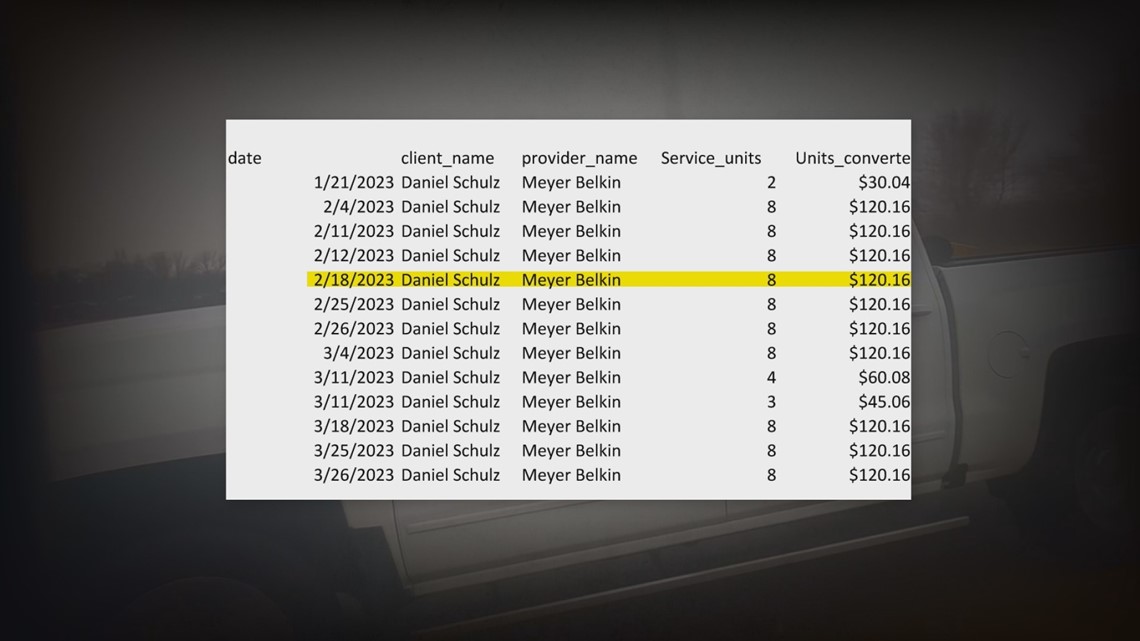
Schulz’s billing records show Belkin billed Medicaid $120.16 on three different instances claiming he was mentoring Schulz by taking him to Whole Foods to pick up food donations.
There are 10 other instances Belkin claimed to have provided peer services to Schulz, but in the billing records Schulz got from Kyros didn’t give an explanation of what service was provided. They all happened on Saturdays and Sundays and totaled $976.
Schulz shared text exchanges he had with Belkin that indicate at least some that billing was also for the grocery runs and appears to constitute inappropriate group billing.

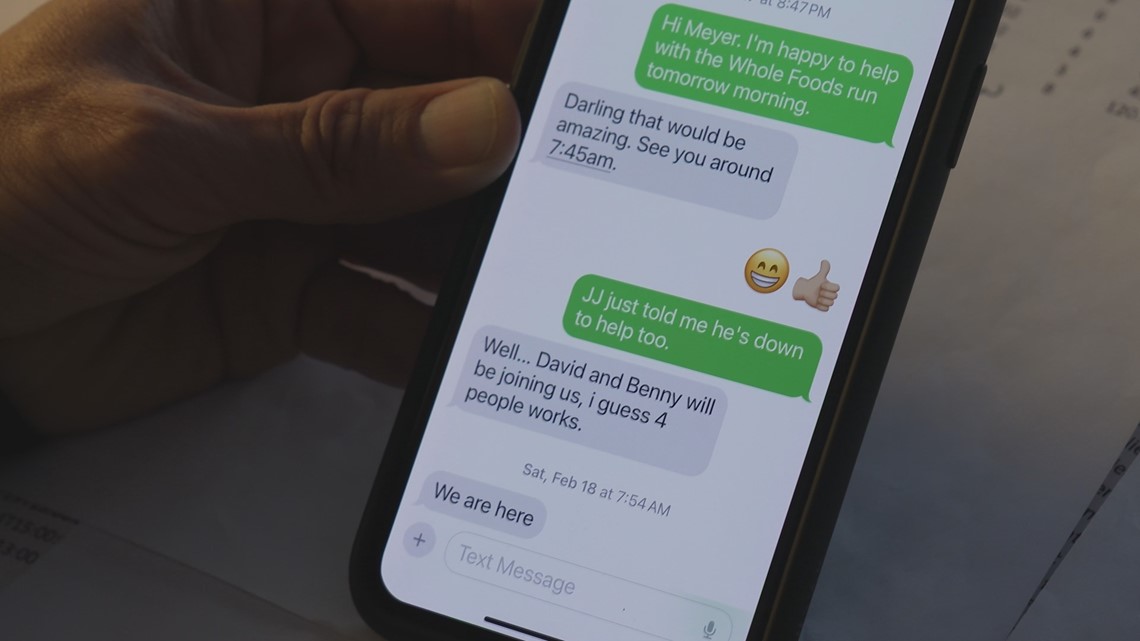
Remember, state law requires peer services be provided one-to-one; group billing is not allowed.
On February 18th Daniel’s records show Belkin billed Medicaid $120 dollars.
Daniel has texts that show when Meyer asked him, he agreed to help Meyer that day with a Whole Foods run. To which Meyer responded, “Darling, that would be amazing. See you around 7:45am.”
The texts show the two discussed how three other sober home residents were also joining them.
In prior reporting, former Kyros peer Ruby McNiff explained how a Kyros supervisor instructed her to bill for groups of people by falsely documenting she had a series of back-to-back, one-on-one meetings.
Belkin declined multiple interview requests, but in response to questions about whether he improperly billed for the grocery runs, he wrote in an email to KARE 11, “...that recent revelations regarding back to back billing have been made...”
He continued, “We immediately stopped that practice. Prior to that we had been led to believe that it was witjin [sic] the ethical billing practices … and our charting was supervised by Kyros.”
When asked about Belkin’s group billing for the grocery runs, Kyros wrote in a statement to KARE 11 reporter A.J. Lagoe, “As an investigative reporter, we would direct you to familiarize yourself with industry standards widely recognized and established by SAMHSA (Substance Abuse and Mental Health Services Administration). This approach would ensure a more balanced and accurate perspective, rather than drawing inferences and conclusions that might only support a predetermined narrative for your story.”
KARE 11 found nothing in SAMHSA standards that says peer services time spent with a group of individuals should be billed to Medicaid as if there were a series of back-to-back, one-on-one meetings.
Chapter 9 Missing Records
Schulz wanted to know what else Medicaid had been billed for in his name so several months after moving out of Belkin’s sober home he went to the Kyros office in Minneapolis to demand his records. After signing release forms, he waited nearly a month.
Minnesota law requires patients be provided their medical records within 30 days.
On day 29 he was informed by Kyros Chief Compliance Officer and General Counsel Kathleen Finnegan, a former Ramsey County prosecutor and top attorney at the Minnesota Department of Commerce, that his records were ready, and he could come the next day and pick them up.
Schulz said Finnegan met him in the lobby and handed him an envelope with those printed pages from a spreadsheet he needed to lay out on the floor.
“Like this is crazy,” Schulz said. “It’s like a jigsaw puzzle.”

“That in my view violates, at the very least, the spirit of the law,” said Brandon Thompson, one of the Twin Cities’ leading medical malpractice attorneys.
KARE 11 asked Thompson to review the records Kyros provided Schulz.
“They were almost incomprehensible,” he said. “The goal here is to make it so it’s easy for people to read, not so they have to print stuff out and put together some jigsaw puzzle and tape it together on the floor.”
He pointed out that Minnesota’s Patient Rights law mandates the release of “complete and current” information “in terms and language the patient can reasonably be expected to understand.”
Kyros has declined repeated interview requests. In a statement, the company wrote, “Kyros provides clients with a complete copy of their medical records in a timely manner in compliance with state and federal law …”
The records given to Schulz are obviously not complete.
In addition to sentences cut off in the middle of words, some entries had no description of what service Schulz allegedly received to justify billing Medicaid.

Kyros sent KARE 11 the following statement:
"All of the data captured in the electronic medical record is available in the Excel spreadsheet. We have not previously heard complaints from clients that information provided to them was missing or was cut-off when printed. If any client information was cut off due to formatting when printed it was certainly not intentional.”
While Kyros said they have not had any complaints, Schulz showed KARE 11 emails in which he specifically requested the company provide the missing information.
It’s been nearly three months since those emails were sent and Schulz says he has not gotten a response or the missing records.
“They’re a software company,” he said. “This is in a computer. I would hope that someone at a software company can figure out how to take that data and push it to a printer and have it print out on paper so the end client can actually get access to their information.”
“It doesn’t seem to me like there is any oversight, regulation,” said Schulz. “Like, who has eyes on this stuff?”
Lawmakers are now asking the same question.
“Does DHS need to reopen their investigation?” asked KARE’s Lagoe.
“They need to have an investigation,” replied Sen. Abeler. “It’s time for DHS to act – and to not act is to fail in their mission.”
DHS declined KARE 11’s interview requests and instead sent a statement reading in part:
“DHS takes oversight of taxpayer dollars very seriously and has strict processes in place to investigate when allegations of improper billing arise … We continue working to improve peer support systems and program integrity oversight of these systems in order to ensure Minnesotans are receiving the best possible care.”
WATCH: KARE 11's original investigation from Dec. 2023:


