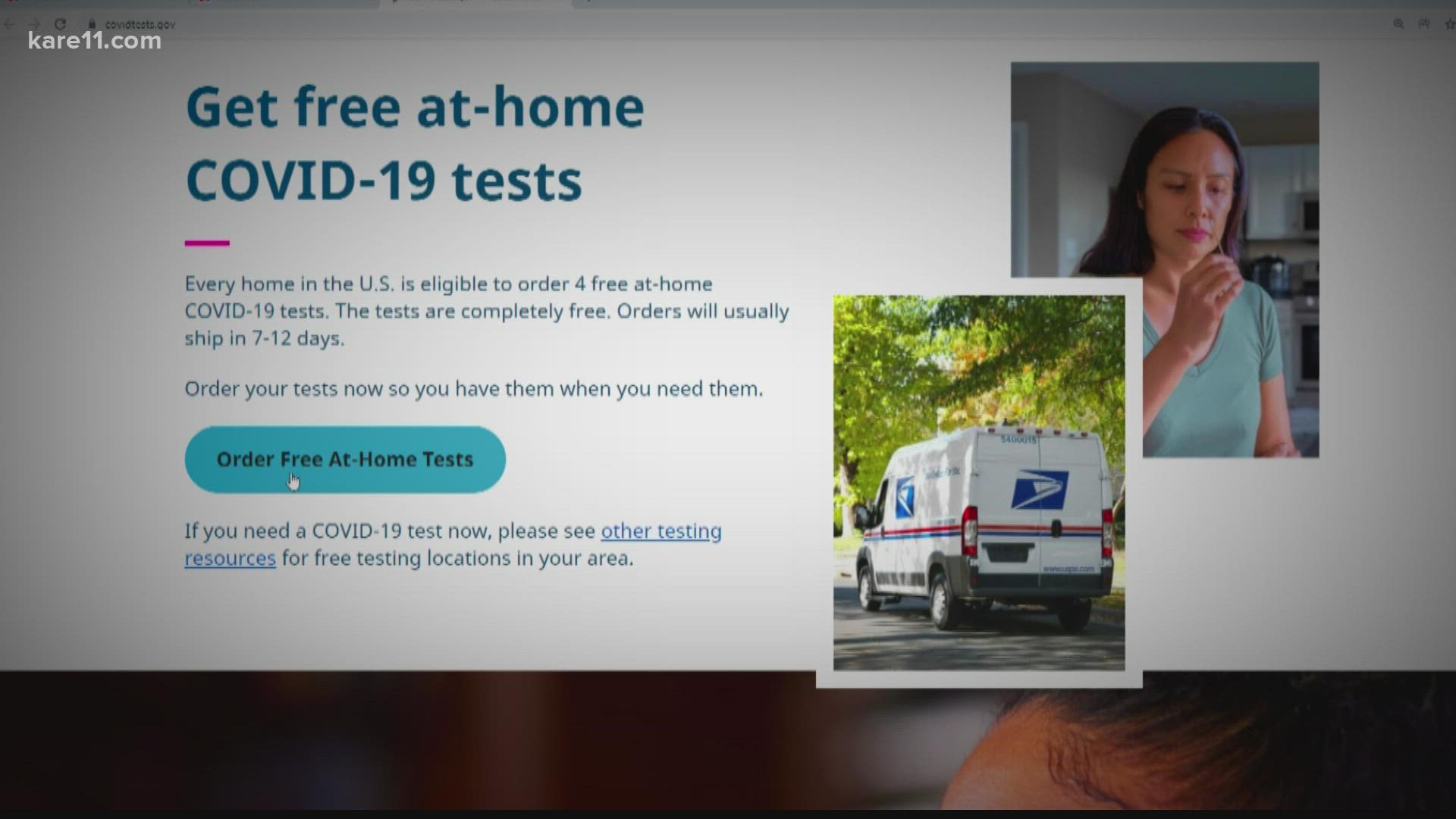
MINNEAPOLIS — Good news, covidtests.gov is live, and Americans are now eligible to order four free at-home rapid tests and have them delivered via USPS. The process is perhaps even easier than ordering something from Amazon.
You hit a button that says "Order Free At-Home Tests" and it redirects you to a USPS site. From there, you fill out your name, your email and your home address and hit check out.
That's it.
You're promised four free COVID Tests from the government that they say will be shipped out at the end of the month. No insurance or payment needed.
Jonathon Hess of Athos Health, a healthcare navigating company says it doesn't get any easier.
"Four free tests, delivered by the United States Postal Service, to every household, or valid home address in the U.S.," he said. "If you have a family of five like I do, you only get four tests."
Which brings us to the next point. Someone in a situation like Jon, would have to then go out and buy more tests for his family.
The Biden Administration said with this testing promise, insurance companies will reimburse Americans for their at-home rapid tests they've purchased from pharmacies.
"That is, if you don't have Medicare, Medicaid, or TRICARE, which is military insurance, insurers have to reimburse everyone on your plan up to eight tests per month," Hess said.
Hess says the reimbursement number of eight is SEPARATE from the four free delivered through the mail.
So using his family of five as an example, with the four from USPS, and his five family members covered under market insurance, Hess would be able to buy and get reimbursed for 40 additional tests.
So this month, he could end up with 44, total, if he wanted.
The reimbursement though would only be up to $12 per test.
"I can buy 40 tests and get reimbursed up to $12 a test for it, my case it would be $480," he said.
That being said, all these tests are at-home rapid antigen tests.
"These tests, as far as I know, do not meet any mandates, they have to be a lab-based test," Hess explained. "So if you want to get a PCR test through the State of Minnesota, which is still free, that would qualify, because that's lab based. Anything that is self administered is not."
However, they're good to use before gatherings or attending school or work to mitigate the spread.
And in terms of the reimbursement process? Every insurance company will have different guidelines.
"There's some general guidelines I can tell you, you're gonna have to fill out a form, take your receipt, put them together, either take a picture and upload it to the website, mail it in or fax it in," Hess said. "Besides that there's not much I can tell you because every health plan has a different thing."
Here are a couple of insurance companies we reached out to with their specific instructions and FAQ pages.
AETNA - COVID FAQ Page (will be updated throughout the week with more information)
UCARE Statement:
"Members of UCare Individual & Family health plans can obtain up to 8 FDA-authorized at-home COVID-19 tests per member per month at no cost (for tests purchased January 15 and after). If a member presents their UCare ID card at the pharmacy counter of a UCare network pharmacy, they will not be charged. If a member purchases a test at a retail store or online, they may submit a Claim Reimbursement Form with their receipt and test boxes to be reimbursed the lesser of the actual cost or $12 per individual test. Because we are in the process of implementing the pharmacy solution, we encourage members to save their receipts and test boxes for reimbursement if their pharmacy is not yet processing the purchase at no cost."
Watch more on the coronavirus:
Watch the latest reports and updates on the coronavirus pandemic in Minnesota with our YouTube playlist: